Joe Soel, author of The Broken Mirror of Memory: Iraq and Other Tales, provides insight into the veteran experience, emphasizing the significance of moral injury, a lesser-known but impactful aspect of military service. As a veteran who served 13 months in Iraq, Joe began writing as a means to process his experiences, eventually turning his reflections into a powerful memoir. He discusses the challenges of reintegration into civilian life, the psychological toll of combat, and the often overlooked emotional and moral struggles veterans face.
Joe passionately argues for a broader recognition of moral injury, which he believes is as crucial as addressing PTSD. He highlights how societal glorification of military service can obscure the real consequences of war, both for soldiers and civilians. Soel explores how the media’s portrayal of military actions can shape public perception and policy, often neglecting the long-term effects on veterans. Through this heartfelt conversation, Soel calls for a deeper understanding and support for veterans, advocating for peace and a more compassionate approach to conflict resolution.
Are you a Veteran interested in receiving peer support? Search for the peer that’s right for you with shared military experience.
Click here for the episode’s full transcript
Make sure you never miss an episode of Reduce The Stigma by subscribing on your preferred platform
How to Watch

Watch on any device on ReduceTheStigma.com

Watch all Episodes on Straight Up Care’s YouTube channel
How to Listen

Our Podcast Website on Podops!
Listen on Apple Podcasts!

Listen on Spotify!

Listen on iHeart Radio!
Listen on YouTube Podcasts!
Follow Straight Up Care
Transcript
Whitney Menarcheck | she/her (00:00)
Americans have two days dedicated to those who have served our country, Memorial Day and Veterans Day. And today’s guest illuminates for us the importance of remembering these individuals every day of the year. Get ready to be inspired as we reduce the stigma.
Whitney Menarcheck | she/her (01:28)
Hello and welcome to Recovery Conversations. Today’s conversation is with Joe Soel, author of “The Broken Mirror of Memory: Iraq and Other Tales.” Welcome, Joe. Thank you so much for joining me.
Joe Soel (01:40)
Thanks so much for having me on, I appreciate it.
Whitney Menarcheck | she/her (01:42)
Yes, you know, I’ve read your book and I really enjoyed it. And I’d love for our audience to hear in your own words what your book is and a little bit about you.
Joe Soel (01:53)
My book is an attempt to get all of Iraq out of me and write it down. And that’s what I really… Well, when I started writing I didn’t know that it would be a book. I thought I was just writing stuff down. And eventually I wrote so much down that it became a book.
Whitney Menarcheck | she/her (02:10)
Yeah, and in the book you wrote about how writing, it sounds like, was always a part of your life. It just was something that maybe was a hobby.
Joe Soel (02:20)
Mm -hmm. Just a hobby.
Whitney Menarcheck | she/her (02:23)
And so you started writing about it and it became a book to get Iraq out of you. That is a very powerful statement. Can you share with us kind of what it was like before you started the process of writing?
Joe Soel (02:39)
It was messy and it was messy throughout the process of writing. It was not a clean sort of walkthrough, shall we say. It was very messy.
Whitney Menarcheck | she/her (02:53)
Okay, and for those who haven’t read your book yet, could you share with us how long you served in Iraq and maybe then how long until you started the process of writing your book after you were released from service?
Joe Soel (03:08)
I started writing in Iraq actually, started writing things down. I served in Iraq for 13 months.
Whitney Menarcheck | she/her (03:15)
Okay. And so you came home and started then just continue, or I should say continued to write from what you had started. And you know, it’s interesting to hear that you started writing over there because I imagine you don’t get many opportunities while on active duty to be in a vulnerable space. How did that come about for you?
Joe Soel (03:41)
It was after a particular attack that I started writing things down. It was during a three -day period with no sleep for me.
Whitney Menarcheck | she/her (03:51)
wow. I’m sorry to hear that. And so in writing this book or writing in general, you came to a conclusion at some point to then share it with, you know, all those who come across it. Can you tell us about what led you to decide to put it out there for others?
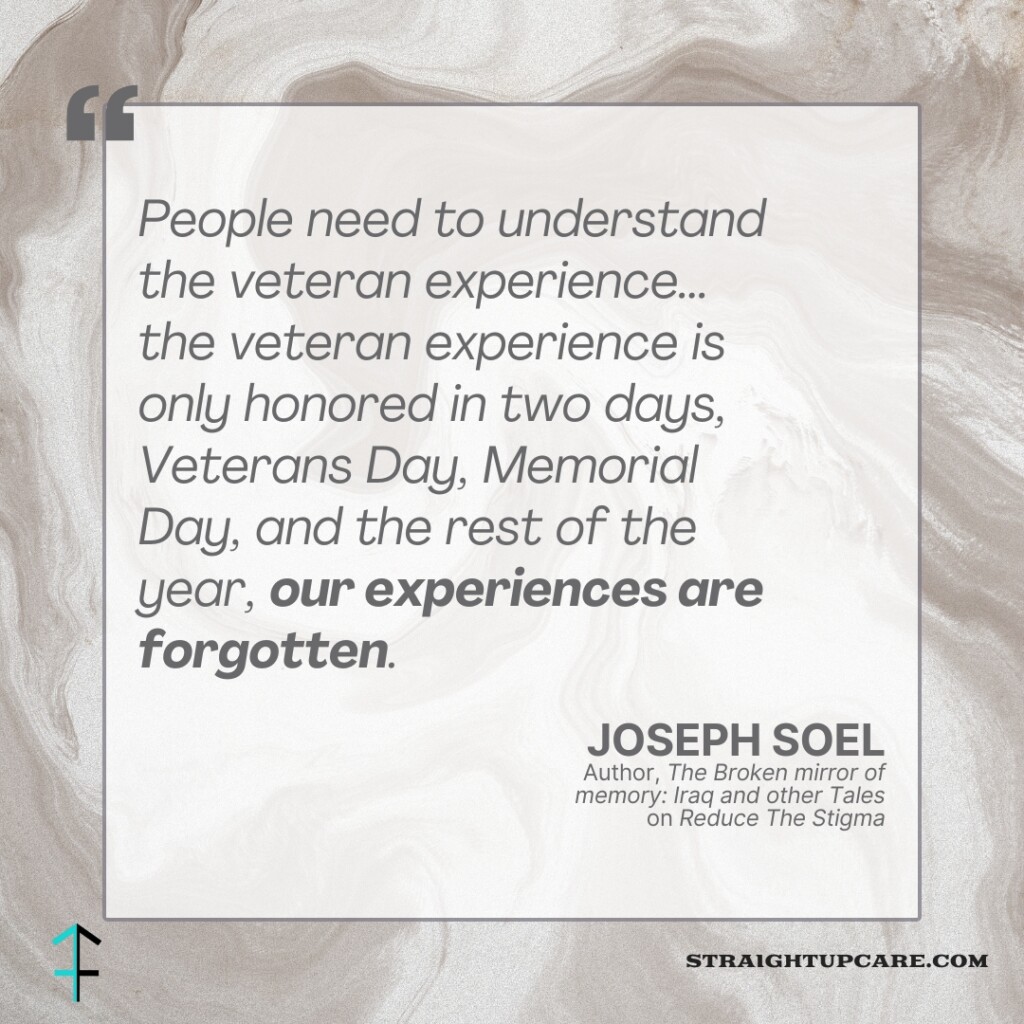
Joe Soel (04:12)
Well, people need to understand the veteran experience. I know, you know, that Memorial Day is coming up, but really, it’s really, you know, the veteran experience is only honored in two days, you know, Veterans Day, Memorial Day, and the rest of the year, our experiences are forgotten. And I feel like on Veterans Day, Memorial Day, they’re paid a lot of lip service by public officials, but it’s not really truly understood. So I wanted to get the story out there so that perhaps we could have less wars in the future. You know, that might be a good thing. And if we have to, we should really think about why we’re going in and what we’re doing and how we take care of the people that we send in when they come home.
Whitney Menarcheck | she/her (04:58)
Right, and your story was a result of the September 11th attacks, if I recall correctly. And I imagine there were many young men and women similar to you, and I’m curious if in retrospect, the publicizing of September 11th, the constant media coverage, if that…
Joe Soel (05:06)
I mean, yes. Yep.
Whitney Menarcheck | she/her (05:26)
played a role in people enlisting and maybe who wouldn’t have otherwise.
Joe Soel (05:34)
I’m certain that it did. It was, you know, as you likely remember, it was wall -to -ball media coverage. So I wouldn’t be surprised if the level of media coverage did contribute to the influx of enlistments. I think that a lot of kids who were in high school like myself during September 11th signed up as soon as they could right after. There was probably two or three from every high school in America you know, at the very least. I’ve heard estimates of 5 million total, something like that.
Whitney Menarcheck | she/her (06:15)
Yeah, absolutely. And that’s a young age to go and serve, whether you’re a reservist or someone looking at active duty and over in a war zone. And so you’re talking about helping people understand the veteran experience. What role does media play on that component? We saw it leading in. We see it in coverage of the war. We saw it in the you know meetup with the September 11th attacks what about the role of media for the veteran?
Joe Soel (06:53)
For the veteran, I think media, much like public officials, pay a lot of lip service to the, What I think my history professor would have called, probably what I would call the American civic religion. And we certainly do have one in this country where there’s a glorification of revolutionary government, which of course our government was founded through a revolution, therefore it is a revolutionary government. We have an example painted on the Capitol Dome of the Apotheosis of Washington. The deification of Washington, he’s in the middle, dressed as a Greek god, that sort of thing. And it really…I’ll let my dog in here. It really tends to grow this culture of the glorification of military service, the glorification of warfare and militarism, and with no real thought of the consequences of that, no real concern for the consequences of that. And in doing so, we’ve set up many millions of soldiers throughout our history, including in the most recent generation, for a lot of suffering and a lot of, you know, we say in the army, you know, you’re setting yourself up for failure. Well, that seems to be exactly what we’re doing with our media coverage of veterans issues and the lead up to the war. If you remember, CNN was a big cheerleader for the war, as was Fox News. And also MSNBC, they cheerleaded us into the Iraq war. And now you can’t find a single anchor probably on Fox News, well, maybe Fox News but you can’t find a single anchor on CNN or on MSNBC that would say, yeah, you know, that was a good decision. You can’t find a majority of the American public that would say, yeah, that’s a good decision to go into Iraq. But at the time, they were all cheerleading for it.
Whitney Menarcheck | she/her (08:47)
Right. So thinking of the individual who served, who’s gone through training, which is physically, mentally exhausting, I can only imagine, what then is it like? What are we not recognizing for that person who returns home?
Joe Soel (09:09)
When you go into the army, you go through basic training, you are trained to be a killer. And when you come to attention, you shout, kill! When you run, you’re singing cadences about killing, and death and destruction, and you’re gonna bring death upon the enemy, and there are even cadences about killing civilians during military training, which is against the Geneva Conventions, not explicitly. And it is explicitly taught in the training classes that you cannot kill civilians, you can’t violate the laws of war. However, the cadences seem to indicate a cultural attitude of almost indifference. While I was in Iraq, I did see a bit of indifference towards civilians. I also saw quite a bit of care from folks in my unit. So…It’s simply reprogramming that then leads to…it leads to a disconnectedness with civilian society when you return. Really the military is what sociologists would call a total institution. So it’s quite similar to a monastery or a prison, except in the case of a monastery it’s not ignored. In the case of a prison it’s not shameful. It’s in fact glorified. So it’s a total institution that is glorified in our society. And it separates you off from the rest of society and it becomes very hard to reintegrate whether you go to combat or not. Combat just makes it worse because that’s the application of the philosophy of the total institution of militarism that exists within our society. When you participate in the application, you are forever changed one way or the other, whether you want to be or not. So that’s really the problem with reintegration.
Whitney Menarcheck | she/her (10:56)
The reprogramming, that word really stands out to me. And what, can you paint the picture for all of us who have not had this experience, for what it’s like when your identity is no longer solely based in your military service?
Joe Soel (11:21)
when your identity is no longer solely based on your military service. I personally became very lost, disoriented. I still continue to strive from goal to goal, achievement to achievement, and still have that military drive which really is all that you…Half left, really, is the drive, but you don’t know what the goal is. You no longer have the mission that you had.
Whitney Menarcheck | she/her (11:52)
Then having to find that new purpose almost in civilian life, while also having gone through an experience that it in some ways it sounds like makes you go against who you would rather be with whenever it’s, you know, pushing kill in these different mindsets. So then there’s that, who am I afterwards? Is that accurate?
Joe Soel (12:21)
Yes, and a lot of it is tied up in the concept of moral injury. When you do things that are contrary to your own deeply held personal beliefs, whether religious, moral, or otherwise. And war will make you participate in things that are distasteful, and you then have to grapple with that and deal with that. So the reintegration is very difficult when you are dealing with doing things that go against your conscience. That’s really what came to mind when he asked the question was really moral injury. What’s the what’s the what’s the disconnect? What’s the difference? What’s What’s the real issue and I think even more than PTSD, which is a real? A real issue. I think moral injury is an even bigger issue, but it’s not very well addressed because that would go against the glorification of the military through American civic religion it would go, you know to say well our soldiers have participated in something that has morally injured them would indicate an error on the part of the system which would then call into question the system therefore moral injury is not very well dealt with and I think that’s a symptom of the glorification of militaristic culture.
Whitney Menarcheck | she/her (13:40)
I mean, you hit it so perfectly. We are all well aware of PTSD for veterans. The statistics, which I cannot rattle off the top of my head, however, we all know it’s outstanding. And moral injury is not something I at least have heard in relation to serving and the veteran experience. Is there…I mean, you just said there isn’t really recognition of it, but is there any space in which it is recognized? Do you even see that amongst your fellow veterans where there’s a recognition of that moral injury?
Joe Soel (14:20)
I do among some of them. Some of the more pro -peace veterans, some of the more peace activist circles that I would travel in. Whereas in the general veteran population, it’s suppressed by drinking, it’s suppressed by new drugs, it’s suppressed by the epidemic of veteran suicide, you know, 22 a day. I…I would be willing to bet that if you did a psychological study, if you drew it out over five years, you would find a lot of those veterans had symptom of moral injury. Now the VA does have programs for moral injury now. They didn’t in 2009. The Army certainly didn’t, and I’m not sure what they’re doing nowadays for that since I’m out of the Army. I’m no longer…
plugged into the institution, shall we say. But I think that as our society progresses a little further, we’re finding that moral injury is being a bit more well treated. It’s hard to acknowledge it from a military standpoint, even speaking with senior members of my former unit when we talk about certain things that I…will not state or bring up and describe when I say, wow, you know, that particular incident really bothered me. And it’s, well, you know, we had no choice. You know, you got to do what you got to do. It is what it is, that sort of thing. That doesn’t make those senior leaders bad or wrong, but they’re dealing with it in a way that they can deal with it. And you can either acknowledge it and…suffer or you can say well it was what it was we do we had to do and you know go on with it and there’s a certain truth to saying we did what we had to do because in many cases it was either you know, fire the missile or you know, continue taking fire, that sort of thing.
Whitney Menarcheck | she/her
And so thinking of, you know, that’s wonderful that there’s starting to be some recognition of moral injury. I can’t help but think about what all we as the people around you, the people in this country, we need to be doing to better support our veterans. And perhaps it is more recognition of the moral injury. Is there anything else that the person who wants to show respect and appreciation to a veteran, what they can keep in mind whenever maybe trying to display that appreciation?
Joe Soel (18:08)
It’s, it’s… I think going beyond thank you for your service as a platitude would be nice. I think the best thing the American public could do, in my opinion, is get out in the street and demand an end to these endless wars, one way or the other. Right now we’re fighting a proxy war in two locations. We’re giving weapons to Israel, we’re giving weapons to the Ukraine to fight Russia.
The Russian army is made up of mostly conscripts. And so those conscripts don’t necessarily want to be there yet. They’re being slaughtered, you know, wholesale by weapons we gave Ukraine. There’s a lot of civilian deaths in Gaza that bother me. Although I will say that the attacks of October 7th were just absolutely horrifying. And I believe some response would have been necessary. Sometimes you have to go to war, it’s a question of how you conduct it. I think that our country should really view war as a very last resort. And when we don’t do that, we expose millions of young men and women to trauma. And we expose, you know, in the case of Iraq, nearly 5 ,000 to death. I think it’s closer to 8 ,000 if you factor in Afghanistan. It might be 7 ,000. But, you know, those are young lives that aren’t coming back. So what the American people could do is demand an end to the system of organized warfare. That’s something that I’ve argued for since I was an undergraduate, is simply defunding, de -escalating, and de -legitimizing the…system of organized warfare that we have as a species entirely, not just as a country, but we seem to have it as a species, don’t we? And I think it’s very troubling that we choose to settle disputes in that manner when you would think there would be such a better way.
Whitney Menarcheck | she/her (20:17)
You think about how different our world is today than hundreds of years ago, and yet we are solving some conflict in the same manner. And the long -lasting repercussions is what really stood out to me when I read your book was the, and maybe this isn’t a surprise to anyone, but just the weight that you carried home with you metaphorically, of course, just the lives touched, the lives lost, the trauma, the impact on you, and while it may be recognized, I’m not sure it’s always truly appreciated. You know, you’re home, so your home be happy, I imagine. You’re shaking your head.
Joe Soel (21:12)
Yeah, and there’s a lot of truth to, hey, you know, your home, be happy. But it’s hard not to get sucked into that black hole.
Whitney Menarcheck | she/her (21:20)
Yeah. And I imagine, you know, you mentioned unfortunately the average 22 lives lost a day of our veterans of our armed services. And that is those who, who we can’t help anymore, unfortunately. There are still many who are affected by you sharing your book about drinking. There are other ways that people are suffering as a result. And by no means is this disrespect or a dismissal of the appreciation of service. It’s just what can we continue to do and how do we continue to support and recognize. What are some ways that you have found to…I don’t know if I want to say make peace. That’s the wrong word. But what have been helpful for you? What do you do to continue moving forward?
Joe Soel (22:17)
I continue trying to do good things for others. I try to build a more peaceful world in my community. I try to serve my church. I try to continue on the process of making amends. You know, there’s a, there’s a Linkin Park song, you know. I’m curious how you’re going to go about making amends to the dead. Actually, it’s Perfect Circle but that’s something, that’s a lyric that’s always stuck out to me. And really, all my life is now is I’m making an amends to the dead and continuing to strive on for them and continuing to just try to do the best that I can to honor them through living a good life, really. And trying to keep that in the forefront of my mind, which is not always possible and not always done. But…it’s something you have to try to do. When you’ve been so close to it, you become very affected by it. At least some people do. Some people don’t. Some people come back and they’re just fine, frankly. But for many people, it is not that way.
Whitney Menarcheck | she/her (23:38)
Great. Great. I am just really touched by your vulnerability in the book and your willingness to speak openly about your experience, recognizing that there is a message of stoicism, you know, for serving. And I think that by sharing your story, you’re really helping everyone gain awareness of the
Joe Soel (23:46)
Thank you.
Whitney Menarcheck | she/her (24:10)
the toll that’s taken as well as what we can be doing. And as we wrap up this conversation, I’m curious if people could walk away with only one message from this conversation, what would you like it to be?
Joe Soel (24:31)
My message would be to love your neighbor as yourself. And when we love our neighbor as ourselves, when we take into account the Lord Jesus’ golden rule, we know that we cannot harm any other being. Therefore, we should be working for peace, we should be loving, we should be kind, and we should take care of our fellow human beings. We’re kind of stuck on this planet together, we might as well get along.
Whitney Menarcheck | she/her (25:04)
Well, I hope everyone hears that because we could all use more kindness in our lives, more joy, and just connection to others. And so thank you so much, Jo, for your book, for your advocacy, and for coming on and talking with me today.
Joe Soel (25:26)
Thanks so much, my pleasure.
Whitney Menarcheck | she/her (25:27)
And if you are interested in learning more and reading Joe’s book, be sure to check it out. It can be found online. It is, again, The Broken Mirror of Memory, Iraq and Other Tales. Thank you all so much for listening.