Mental Health and Substance Use Battles for Veterans
For many veterans, the battlefield they face is within themselves—a complex terrain where mental health challenges and substance use disorders intertwine, creating a formidable adversary to their well-being. Understanding the prevalence of these issues among veterans is crucial for providing effective support and care for those who have served their country.
The statistics paint a devastating picture. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), around 20% of veterans who served in Iraq and Afghanistan suffer from post-traumatic stress disorder (PTSD) or major depression.
Moreover, the prevalence of substance use disorders among veterans is significantly higher than in the general population, with alcohol and prescription drug use being particularly common.
Combat exposure, multiple deployments, and the stress of military life contribute to the development of mental health disorders among veterans. PTSD, in particular, can manifest through intrusive memories, hyperarousal, and avoidance behaviors, making it challenging for individuals to reintegrate into civilian life. To cope with these symptoms, many turn to substances such as alcohol, prescription medications, or illicit drugs as a means of self-medication.
While statistics specifically focused on non-combat veterans might be less prevalent compared to those for combat veterans, research suggests that mental health issues and substance use disorders are still prevalent among this group.
Factors such as the stress of military service, deployment-related experiences, transitions to civilian life, and exposure to traumatic events can all contribute to mental health challenges and substance use disorders among veterans, regardless of whether they saw combat.
According to the U.S. Department of Veterans Affairs (VA), approximately 11-20% of Operation Enduring Freedom and Operation Iraqi Freedom (OEF/OIF) veterans (which include both combat and non-combat veterans) experience post-traumatic stress disorder (PTSD) in a given year. Additionally, substance use disorders are common among veterans, with rates varying depending on the substance and other factors.
While specific data on non-combat veterans may be somewhat limited, it’s clear that mental health and substance use disorders are significant issues that can affect veterans regardless of their combat status.
The relationship between substance use and mental health among veterans is complex and multifaceted. Substance use can exacerbate the symptoms of underlying mental health disorders, leading to a vicious cycle of self-destructive behavior. Conversely, individuals with substance use disorders are more likely to experience mental health issues such as depression and anxiety.
Access to adequate care and support for veterans struggling with these challenges is critical. Unfortunately, many barriers exist that prevent individuals from seeking or receiving the help they need. Stigma surrounding mental health and substance use disorders within the military culture can deter service members from acknowledging their struggles and reaching out for assistance. Additionally, limited resources and long wait times within the Veterans Health Administration (VHA) can hinder access to timely and appropriate treatment.
Addressing the complex needs of veterans requires a holistic approach that integrates mental health services with substance use disorder treatment. Early intervention and comprehensive assessment are essential for identifying and addressing co-occurring disorders effectively. Evidence-based therapies such as cognitive-behavioral therapy (CBT) and dialectical behavior therapy (DBT) have shown promise in treating both PTSD and substance use disorders concurrently.
Moreover, peer support programs and community-based initiatives play a vital role in providing veterans with a sense of belonging and understanding. Connecting with fellow service members who have walked a similar path can foster a supportive environment where individuals feel comfortable discussing their experiences and seeking guidance without fear of judgment.
Beyond clinical interventions, addressing the social determinants of health is crucial in supporting veterans’ well-being. Stable housing, employment opportunities, and access to education and vocational training can significantly impact veterans’ quality of life and reduce the risk of substance use and mental health problems.
As a society, we have a moral obligation to honor the sacrifices made by our veterans by ensuring they receive the care and support they deserve. By recognizing the complex interplay between substance use and mental health among veterans and implementing comprehensive, evidence-based interventions, we can help them navigate the battlefield within and embark on a path toward healing and recovery.
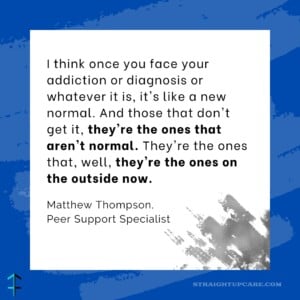
Peer Specialists, Veterans – They Understand
Read the article about Matthew
Triumph Through Struggle: A Marine’s Journey to Support and Healing
Watch Matthew’s full interview
Reduce The Stigma – Meet The Peer: Matthew Thompson
Schedule a peer support session with Matthew
https://straightupcare.org/appointment-schedule/469
Read the article about Ryan
Rising Strong: Addiction, Mental Health and Finding Purpose
Watch Ryan’s full interview
Reduce The Stigma – Meet The Peer: Ryan Spillane
Schedule a peer support session with Ryan
https://straightupcare.org/appointment-schedule/520
Follow Straight Up Care
|
|